Alzheimer's: prevent instead of cure?
Alzheimer’s disease (AD) is a huge public health issue as it affects a large part of the aging population. Neuropathology is studied primarily in the end stages of the disease. What about prevention?
Posted by
Published on
Thu 23 Apr. 2015
Topics
| Alzheimer's Disease | ErasmusLadder | Gait | Locomotion | Motor Learning |

Alzheimer’s disease (AD) is a huge public health issue as it affects a large part of the aging population. By 2050, experts estimate this number will exceed 100 million worldwide. Those of you that are a familiar with the underlying pathological hallmarks of AD will recognize the terms plaques and tangles. These protein built-ups in the brain are well-researched; however, this neuropathology is studied primarily in the end stages of the disease.
Plaques and tangles
Plaques and tangles are discovered in postmortem studies of humans, and in rodent models of the disease. But while these clusters of beta amyloid plaques between neurons and tangles of tau protein inside of the cells have always been prime suspects in AD symptoms, recent studies show that clinical symptoms can appear independently of their onset.
Early onset Alzheimer’s in Columbia
One recent study demonstrating groundbreaking research on AD, was carried out in collaboration with a group of 25 families from the Antioquia area in Colombia. Researchers from the University of Antioquia learned of a high prevalence of early onset familial Alzheimer’s disease (FAD) in these families, which they now know is caused by a presenile1 (PS1) gene mutation. Results from a longitudinal study showed that in this population clinical symptoms appeared as early as at 40 years of age, even before plaques were identified in the brain. These findings might lead to important discoveries in the treatment of Alzheimer’s in general.
Prevention instead of cure
Working together with these families, researchers from the University of Antioquia, the Banner Alzheimer’s Institute, National Institutes of Health, and Genentech are now investigating if, instead of trying to cure or treat the symptoms in later stages of the disease, AD can be prevented or slowed down during the onset phase. Young members of these families that were identified to carry the gene mutation have entered a clinical trial to address this possible area of treatment.
Murine model laboratory research
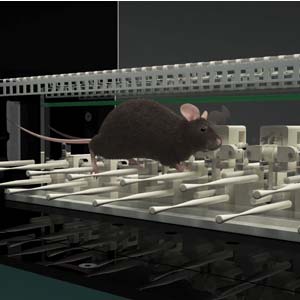
In addition to clinical research, a mouse model of the PS1 gene mutation FAD was studied in the lab by Diego Sepulveda-Falla and his colleagues (The Journal of Clinical Investigation, 2014). Previous research has shown that this murine model develops plaques and tangles in the brain similar to that seen in humans with AD. Using the ErasmusLadder test, which focuses on cerebellar-based motor performance and learning, PS1-FAD mice were found to have deficits in both motor performance and motor learning (see below). Strikingly, these symptoms occurred before amyloid plaques were found in the brain, indicating that the PS1 mutation results in AD symptoms in another (perhaps additional) way than through the “typical” protein build-ups.
Motor performance and learning tests
During the ErasmusLadder task, mice went through two phases of testing. First, motor performance while mice were learning to step across alternating high and low horizontal ladder rungs. An efficient stepping pattern requires use of the higher rungs; usage of a lower rung was counted as a misstep. Skipping rungs, or slower stepping, was also measured. Normally functioning mice learn, over repeated runs, to traverse the ladder quickly and efficiently, indicating good motor functioning. In contrast, PS1-FAD mice exhibited difficulties in this phase as was evident from their longer step times and a higher number of missteps. Furthermore, PS1-FAD mice demonstrated problems with learning when to leave the goal box (as cued by a sound); these mice left before the cue was given or stayed in too long after the cue was given.
In the second phase of testing, a perturbation was introduced on the horizontal ladder. Precisely timed for each individual run, a single rung was raised above stepping level, higher than the previous high level rungs. Cued by a sound, introduction of the obstacle rungs challenged the motor learning abilities of the mice. Again, PS1-FAD mice demonstrated difficulties in navigating this reflexive motor learning task.
PS1 mutation causes symptoms independent of plaque formation
The combined clinical and laboratory studies discussed above suggest that the specific PS1 mutation in the Purkinje cells of these patients from Antioquia is causing symptoms that are independent of the formation of amyloid plaques. Currently, a large group of members from these families are entering into a clinical trial for AD prevention, testing a drug that specifically works to prevent the formation of these plaques. It will therefore be interesting to see if this drug will control any or all aspects of the PS1-FAD pathophysiology, as it appears that these symptoms occur independently of plaque formation. New avenues of treatment may need to be assessed.
Read more
Sepulveda-Falla, D.; Barrera-Ocampo, A.; Hagel, C.; Korwitz, A.; Vinueza-Veloz, M.F.; Zhou, K.; Schonewille, M.; Zhou, H.; Velazquez-Perez, L.; Rodriguez-Labrada, R.; Villegas, A.; Ferrer, I.; Lopera, F.; Langer, T.; De Zeeuw, C.I.; Glatzel, M. (2014). Familial Alzheimer's disease-associated presenilin-1 alter cerebellar activity and calcium homeostasis.The Journal of Clinical Investigation, 124(4), 1552-1567.
Related Posts

A plant-based treatment for Alzheimer's disease?

Mice with Alzheimer’s disease walk well but remember poorly