Extracellular vesicles from umbilical cords improve traumatic spinal cord injury
Spinal cord injury is crippling and hard to treat. Secondary injury caused by inflammation and scarring significantly impact motor function and locomotion. Extracellular vesicles can improve recovery.
Posted by
Published on
Thu 22 Dec. 2022
Topics

Traumatic spinal cord injury could happen to anyone, and it is a very crippling neurological disorder.
Spinal cord injury treatments
Available treatments are not bad, but a group of scientists from Austria and Croatia thought they could still be improved significantly. They developed a new version of a potential treatment, which decreases the consequences of secondary damage after a traumatic spinal cord injury.
Inflammation and scarring
The initial injury triggers inflammation in the body, causing secondary damage. This happens very soon after the injury, so any treatment needs to be applied as soon as possible.
Usually, the local inflammation is maintained by the body, which on one hand helps repairing the damage done, but on the other hand is suspected to block healing. The latter seems to be caused by the forming of fibroglial scarring at the injury site.
Basic treatment with extracellular vesicles
Once someone has received a traumatic spinal cord injury, they usually receive a systemic treatment with a specific type of extracellular vesicles (EVs). These EVs are from human umbilical cord mesenchymal stromal cells (hUC-MSCs). However, it is suspected that this systemic treatment does not work fast enough and that a local delivery of high doses is needed instead.
Experimental treatments
In order to test these ideas, the scientists tested various treatments using a rat tSCI (traumatic Spinal Cord Injury) contusion model. They used 4 groups of 26 female rats each.
One group was the control, the other groups received either a vehicle injection, an EV injection to the lesion site or an EV injection to the tail vein. All groups underwent the same surgery (a laminectomy).
The rats underwent various motor function and locomotion tests, a thermosensitivity test and bladder voiding checks (see paper for the latter two).
Surgery and treatment
All rats underwent a laminectomy, where a contusion was applied to vertebra Th8. Immediately after, all rats (except the control group) received an injection either at the lesion site or in the tail vein. Following surgery and treatment, the rats underwent various tests in order to find out the long-term results of the treatments.
Motor function and locomotion
Following the traumatic spinal cord injury, the researchers tested the rats’ motor function, locomotion and response to thermal stimuli in order to check their neuroregeneration.
Before surgery, the rats had had 4 weeks of acclimatization to handling of experimenters, including 2 weeks of training for the tests. The last training pre-surgery was intended as a baseline comparison.
Mobility
Using a 1m diameter arena, the rats’ BBB-score (0-21) was taken regularly until week 8 post-injury. From being nearly paralyzed, the rats’ mobility improved significantly, with the lesion site EV injected rats recovering fastest after week 2 post-injury.
In another test, conducted once pre-surgery and twice post-surgery, they walked an irregularly spaced horizontal ladder. Each rat walked 3 times, on different ladders, and the missteps were calculated. The EV treated rats performed slightly, but not significantly, better at week 8 post-surgery.
Gait analysis
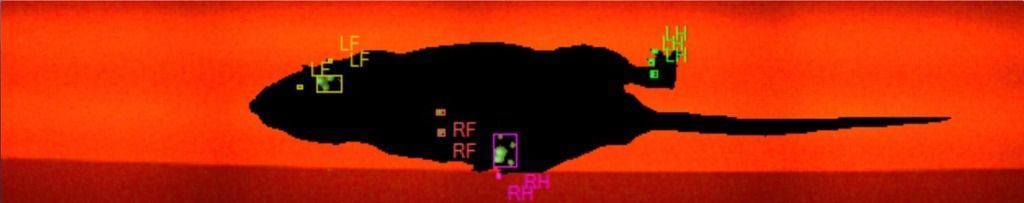
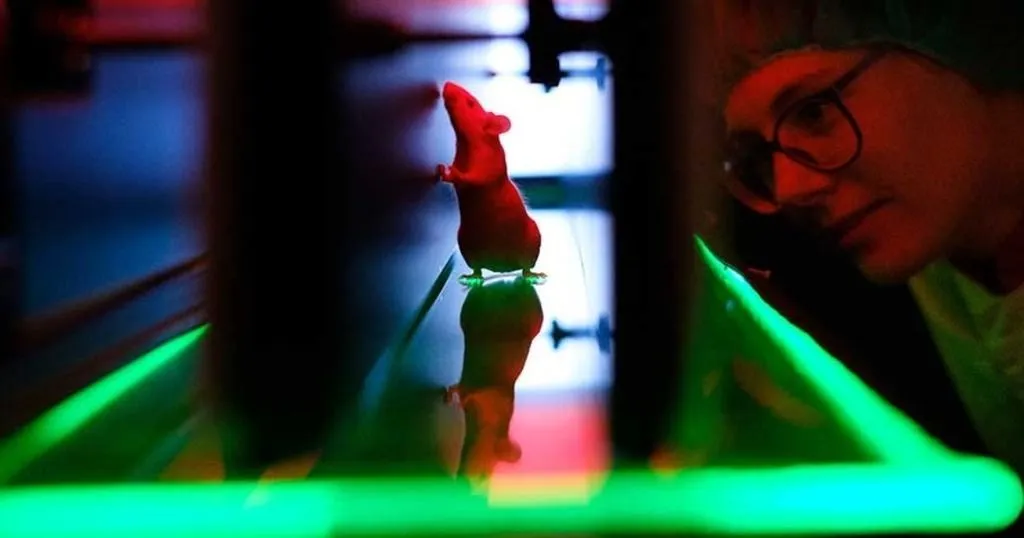
Lastly, the rats’ gait was analyzed, using Noldus CatWalk XT. Apart from gait, the program also analyzed limb coordination. Each rat walked over a glass plate towards a goal box several times. Using the built-in camera, the rats’ pawprints were documented individually and automatically.
The rats had to complete 6 valid runs, meaning walking across the recording window without pause. These tests were done 2 times pre-surgery, and at weeks 3, 5 and 7 post-surgery. Starting from week 5, the lesion site EV injected rats performed, not quite significantly (p = 0.06), better than the intravenous EV injected rats.
Recovery from traumatic spinal cord injury
Rats treated with an intralesional injection of EVs recovered significantly better than the other treatment groups. Especially long-term recovery is improved by this treatment. Generally, both EV treated groups recovered better than the vehicle-treated rats.
Reduction of inflammation and scarring
The researchers found that acute intralesional EV application significantly reduced inflammation during the acute phase post-surgery, and is expected to improve long-term functional outcome. This reduced inflammation is still detectable at day 14 post-surgery, and also helps reducing scarring.
The latter effect was not nearly as strong in intravenous EV injection. However, since post-tSCI scarring in humans develops over a longer timespan, recurring treatment might be more effective.
The most effective treatment for traumatic spinal cord injury
In short, a fast intralesional application of EVs seems to be the most effective treatment. They cause a more robust improvement of motor recovery compared to IV delivery and it is more potent.
Early application reduces inflammation and scarring most. The actual way EVs help after tSCI is not clear yet, but these two effects, and improvement of vasculature integrity, seem to play a major role.
References
Romanelli, P., Bieler, L., Heimel, P., Škokić, S., Jakubecova, D., Kreutzer, C., Zaunmai, P., Smolčić, T., Benedetti, B., Rohde, E., Gimona, R., Hercher, D., Dobrivojević Radmilović, M. & Couillard-Despres, S. (2022). Enhancing functional recovery through intralesional application of extracellular vesicles in a rat model of traumatic spinal cord injury. Frontiers in Cellular Neuroscience, 15, 795008.
Related Posts

How to let rats run perfectly
Assessing gait in a mouse model for Leigh Syndrome

